The appliance of science
Joël Lacey goes behind the scenes with the scientists of Poole Hospital
Published in January ’19

A member of the pathology department’s team of scientists with one of the robotic machines that prepares around 3000 samples a day for nearly ten times that number of tests
The phrase ‘What’s wrong with me?’ is the often unspoken question that leads us all, at some point in our lives, into the medical world. While TV programmes like House or Grey’s Anatomy would have us believe that the right doctor can individually and magically pronounce the cause of our ills and their treatment, that is just not the case in the real world.
To misquote Isaac Newton: ‘If doctors can see more clearly what ails us, it is because they are standing on the shoulders of science.’ Science that would be inaccessible without the help of Poole Hospital’s Healthcare scientists and engineers.
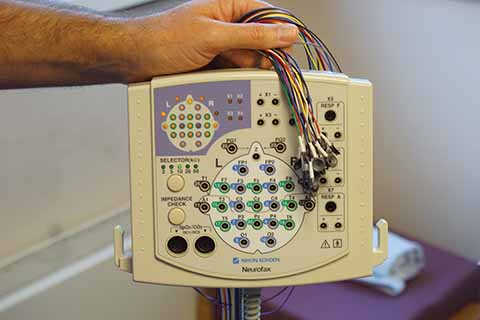
John Flannery holding a bunch of transducers that are attached to the head of patients to measure their brain activity
This is not to denigrate the medical and surgical doctors and nurses and all allied health professionals, rather it is a fundamental acceptance that without the staggering amount of technology available to them, the frontline medical staff would find it much, much harder to diagnose and treat patients.
How much harder? Well with somewhere between 80-90% of diagnoses being based on pathology (blood sciences, cellular sciences and infection sciences) the answer is very much harder. In the 2016/17 year, Poole Hospital’s pathology department conducted 11,004,603 tests. Of these, all but half a million were done in blood sciences, 132,590 were tissue and cell tests and 354,262 were microbiology and virology tests for infection.
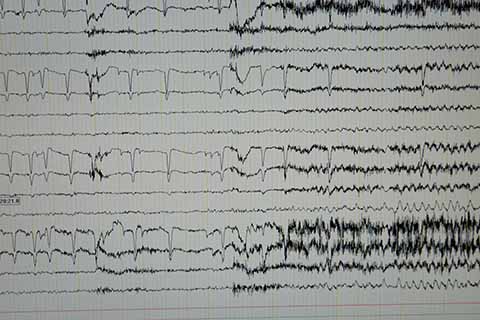
One doesn’t need to be a neurophysiologist to see the point in this trace where a seizure starts, but it takes years of training to understand why it may be happening and what it signifies for the patient
There are 250 Healthcare scientists at Poole Hospital, who all have a degree in their specialist subject. Many roles also require a masters degree and several years of training. There are equivalent to 175 full-time members of staff in pathology, where, according to Mike Trevett in Blood Sciences: ‘Tests are requested based on the patient’s current condition, or treatment. There is a vast array of tests that we offer – around 100-150 in house– and if there’s something outside of this, we can refer it to specialist labs around the country.
‘Within haematology we’re assessing full blood counts; red cells, white cells and platelets and also coagulation screens looking at clotting times . Within biochemistry they offer even more tests looking at chemical pathways, protein markers and tumour markers. We’re not just here to provide a diagnosis of what someone may have, but also to eliminate conditions that they don’t have.
‘This department serves inpatients, outpatients, GP surgeries across Poole and parts of Bournemouth and the private hospital adjacent to this one. In the mornings our main focus is processing samples from inpatients and outpatients. In the afternoon, the bulk of our workload is from GP surgeries. We have a pod system (like the pneumatic systems used in department stores to transfer cash) which connects to the wards and we have an urgent system, so everything from A&E comes into us this way. In all, we receive about 3000 samples a day (on which multiple tests will be performed).

Charlie Martin explaining the way multi-leaf collimators channel the ionising radiation in the treatment of tumours
Tanya Hart, a clinical scientist in the biochemistry section of blood sciences, explains some of the machinery involved: ‘This first line [pictured at top of page] prepares the samples, removes the sample bottles’ caps, prepares the samples for whatever tests need to be performed. Then we have interfaces connected to our medical equipment that then know what tests need to be performed on that sample. It’s all electronically logged and driven. The idea is that we have a lot of big machines that do all the repetitive jobs and then the expertise and training of the scientists can be used to interpret the results of the data from those tests.
‘There are all different types of cancer and some of them have specific blood tests that can help with diagnosis. There are certain types of cancer where blood counts can be greatly affected and then we can also check the blood for certain kinds of marker. For example, ovarian cancer can release a molecule into the blood called CA125.’

Emma O’ Shaughnessy calibrating the Gamma camera, which is used to visualise Technetium-tagged deposits in cancerous cells
It’s not just for initial diagnosis either, as Mike Trevett explains: ‘For cancer patients, anyone who has chemotherapy or surgery may require a full blood count, blood clotting check or a blood transfusion. For those undergoing chemotherapy, you want to check the full blood count, to check their haemoglobin levels are stable, their white blood cell count and their platelets are adequate; they may also have a blood group sample taken and, if necessary, they would be given the right blood products to improve their condition.’
The analyses based on blood samples normally take from 40 minutes to perform, but pathology is not the only place where tests are conducted in Poole Hospital. Bedside monitors for inpatients are constantly checking blood oxygen levels, blood pressure and heart rate and rhythm instantly in real time.
At the other end of the test-length spectrum is the work conducted by Neurophysiology Healthcare Scientist Jon Flannery (and colleagues), to measure nerve and brain function in patients presenting with seizures or other neurological symptoms: ‘One of our tests may last up to 96 hours,’ he explains. ‘I monitor and record nerve function be it in the brain, eye, spine, or limbs.
‘When we do an EEG, Electro-encephalography – electro, we attach electrodes; encephalo, of or from the head; and graph, well, to graph – we’ll attach 24 transducers (electrodes) to our patient’s head to record on-going brain activity. Our patients are admitted to a room with a bed, a microphone and the video camera’. All the information goes into the EEG computer, and is analysed by the scientist and medical team.
‘It’s not a perfect analogy for how the brain works, but if you imagine taking a photograph of an orchestra, you can see what instruments are there, but it’s only when you make a recording that you find out whether they’re playing in tune or not. They may look fine, but sound terrible together. We’re trying to determine whether the brain goes ‘out of tune’ during the patient’s symptoms.
‘We’re asking “what does it our patient’s seizure physically looks like, and how it is the brain working at that time?”. You may come to the end of that 96-hour recording and say, “Well it’s not epilepsy, so let’s go down another diagnostic path; it’s not fainting so let’s go down another path, an MR scan picture may reveal something developing in the brain.”’
Claire Davies is a Medical Physicist in Diagnostic Radiology and monitors the imaging equipment. When a brain scan of a patient is required, initially a Computed Tomography (CT) scan is performed. If further imaging is required it is done using Magnetic Resonance Imaging (MRI) scanner. Computed Tomography scanners use X-rays, an MRI scanner uses a strong magnetic field.
Around 500,000 diagnostic imaging procedures are taken across Dorset each year. Poole Medical Physics department monitors nine CT, eight MRI scanners, 150 X-ray units and fifty ultrasound imaging systems across East Dorset. Healthcare scientists do a significant amount of testing to ensure that the equipment works in accordance with national guidelines. Healthcare scientists do a significant amount of testing and optimisation of the equipment to ensure the lowest dose is given in order to obtain diagnostic images.
Emma O’Shaughnessy, Principal Physicist in Nuclear Medicine, uses radioactive materials in diagnostic, curative and palliative ways. ‘Nuclear medicine is involved with radioactivity that you attach to a drug which takes pictures of different organs in your body depending on the drug the radioactivity is attached to and PET (Positron Emission Tomography – which also has the addition of a low radiation dose CT scan) is the same. So depending on what you’re trying to look at or treat in the body, you use a different isotope and chemical to which you attach it. For a lot of the tests we do diagnostically we use an isotope called Technetium-99m, which is a really good imaging agent. It produces powerful enough gamma radiation to come out of the body, but not so powerful that it goes through all the instrumentation you’re trying to measure it with; it’s also got a relatively low half-life (six hours) so even if you inject relatively large amounts on the day of the image, 24 hours later you don’t have to worry about it.
On the treatment side, as Emma explains: ‘The majority of treatment we are involved with is for thyroid cancers where a very simple radioactive iodine compound will go straight to the thyroid cells and kill cancer cells in the thyroid or anywhere else in the body these cells may have deposited. There’s also a treatment for prostate cancer where you can inject Radium-223 and that’s a very effective palliative treatment and it has also been shown to prolong life.
‘For PET scanning, Fluorine-18 is attached to sugar for most studies so wherever you may have a cancer in the body, as [cancer] is a growing cell, it takes sugar from the blood. With the latest scanners, if the sugar uptake is enough, you can see things as small as a strawberry pip. For bone scans, we attach Technetium-99m to a phosphate analogue which gets taken up by the bone and we can see cancerous deposits on a bone scan much earlier than you might on a CT scan. We also have a treatment called Samarium-153 therapy, which can be used for any cancer where there is pain from a cancerous bony deposit. The effects can be dramatic in terms of pain relief.’
Charlie Martin is a physicist in radiotherapy, where patients tend to arrive at the end of their diagnostic pathway, and normally with cancer: ‘radiotherapy can treat Dupuytren’s contracture, where it is an alternative to surgery to alleviate the involuntary and otherwise normally irreversible bending of fingers, but by and large we deal with cancer.
Radiotherapy works by breaking DNA inside the cancer cells, stopping them from multiplying and killing them.. As technology has improved, targeted radiotherapy and better imaging has made it easier for us to treat. With radiotherapy using ionising beams, you can’t tell the radiation where to stop, so if you were to put a long exposure single beam onto a cancer you’d also be ionising the tissue before and the tissue after the cancer. By using multiple beams from different angles, you reduce the exposure to healthy tissue and focus it more on the cancerous tissue by where it crosses over. We’re using X-rays in a Megavolt range not the kilovolt range that’s used in imaging. We can project the beam from 360 degrees and match the shape from the angle to the shape of the tumour established from the imaging. We do CT scans on the patient before treatment and doctors define the area they want treating. We can treat field sizes up to 40cm but we’re normally treating much smaller areas so we restrict the beam to a rectangular shape using metal shutters and smaller ‘fingers’ called multi-leaf collimators that focus the beam to a specific shape for the angle at which the beam is bring directed – like dodging and burning-in in a photographic darkroom.
The imaging and radiological equipment isn’t the only technology that needs support at Poole Hospital, as Clinical Engineering Manager John Pickett reveals: ‘We support equipment throughout the hospital from thermometers to anaesthetic machines and life support and everything in between, from the moment we have someone say “it might be an idea to get this”, to dealing with it at the end of life and safely disposing of it. We also look at incidents involving equipment to identify faults or potential improvements. We use a database to record all our assets and currently have somewhere shy of 10,000 assets for Poole, there are about 600 models of different pieces of equipment and the last time I counted up, the replacement value was £60,000,000.’
The sheer scale of the testing and the breadth of the science may be breath-taking, but the clinicians and scientists of Poole Hospital are only too well aware that, from the perspective of patients and their families, as Isaac Newton also said: ‘It is the weight, not numbers of experiments that is to be regarded.’

